
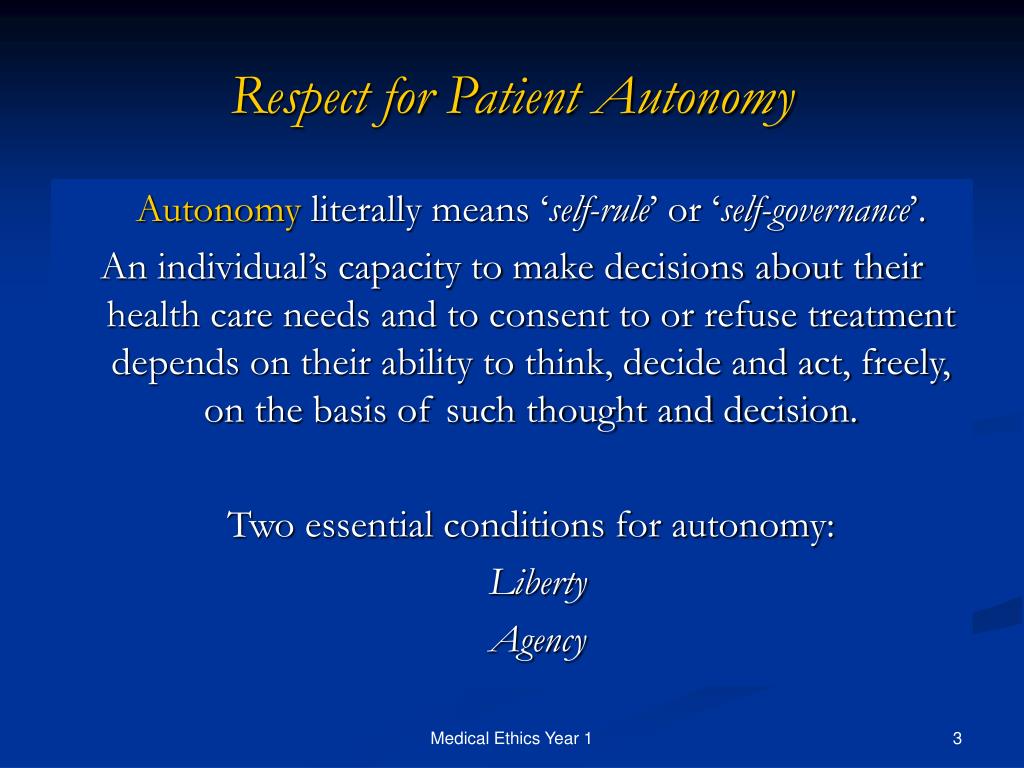
However, nurses are obligated to honor a patient’s autonomous actions. Illness may threaten a patient’s autonomy. Autonomy is the ability to explain one’s needs and make fully informed decisions about one’s health. Nurses must respect their patients at all times, but they’re not required to accept the actions their patients take and the consequences of those actions. Beneficence is exemplified by the kindness nurses show their patients in all their interactions and in the willingness to abide by a patient’s wishes, as long as the patient is competent and fully informed. Beneficence is rooted in the innate love we feel for humanity and the drive to demonstrate that love through our actions. Nurses have a strong duty to act in ways that benefit individuals, communities, and society. Examples of nonmaleficence are always being truthful to patients and never allowing one patient to be harmed for the benefit of another. They must also promote good actions on behalf of their patients. Nurses have an obligation not to inflict harm and not to allow others to inflict harm.


The Oncology Nursing Society describes the principles of nursing ethics that serve as guideposts for ethical decision-making in healthcare settings. Principles of Nursing EthicsĮthical principles are general by nature because they’re intended to serve as a framework that people use to weigh the facts of a situation that presents a moral or an ethical dilemma. This can be especially challenging when the patient and nurse come from different racial, gender, or ethnic backgrounds. Trust is key to ensure that patients are comfortable sharing information about their culture and socioeconomic status with nurses and other healthcare professionals. Nurses should be mindful of the social and economic factors that affect patient and community health. They can then refer patients to social workers, case managers, and other healthcare team members for additional services. To address health inequity factors, nurses are encouraged to be aware of health disparities that could impair treatment outcomes. How Ethics Improve Patient Care Across Demographic Groups
ETHICAL PRINCIPLE OF AUTONOMY IN NURSING PROFESSIONAL
adults surveyed trust the COVID-19 information they receive from doctors and nurses, compared to 73% who trust information from the U.S. A Harris Poll conducted in August 2020 found that 88% of U.S. The trust patients put in their nurses has only grown stronger as a result of the ongoing COVID-19 pandemic. The next highest-rated professions for honesty and ethics were engineers (66%), medical doctors (65%), and pharmacists (64%). residents, 85% of respondents rated nurses’ ethical standards and honesty as “very high” or “high.” That marked the 18th year in a row that nurses received the highest rating in the survey of consumer impressions of various professions’ ethics. At a time of unprecedented change, one constant remains: Nurses rate the highest of all professionals for honesty and ethics.Īccording to a 2019 Gallup poll of U.S.


 0 kommentar(er)
0 kommentar(er)
